On August 4, 2021, the Centers for Medicare and Medicaid Services (CMS) published the final rule in the Federal Register for fiscal year (FY) 2022 Skilled Nursing Facility Prospective Payment System (SNF PPS). The regulations take effect October 1, 2021.
Each year, CMS publishes updates to the regulations for inflation factors, wage index adjustments, and other patient-care related payment adjustments. Below is an overview of the FY 2022 SNF PPS, including finalized changes and other relevant updates.
Key Finalized Changes to SNF Payments
The final rule includes the following key changes:
- A 1.2% payment increase in payments to SNFs
- Code mapping classifications for the Patient Driven Payment Model (PDPM) case-mix
- Updates to the SNF Value-Based Purchasing (VBP) Program
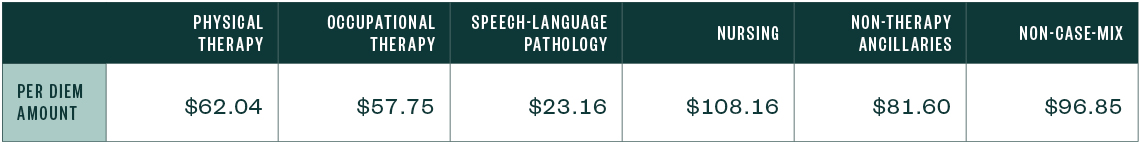
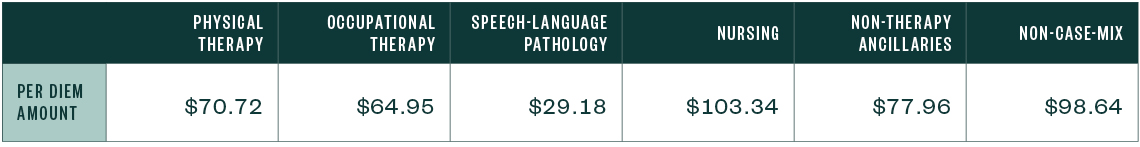
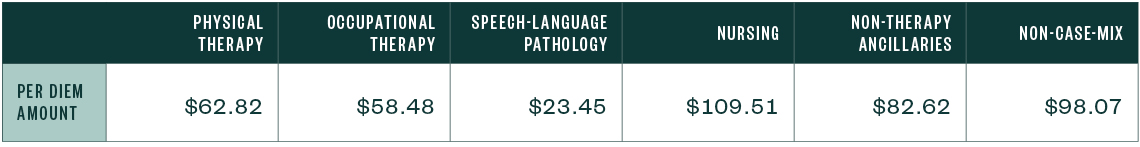
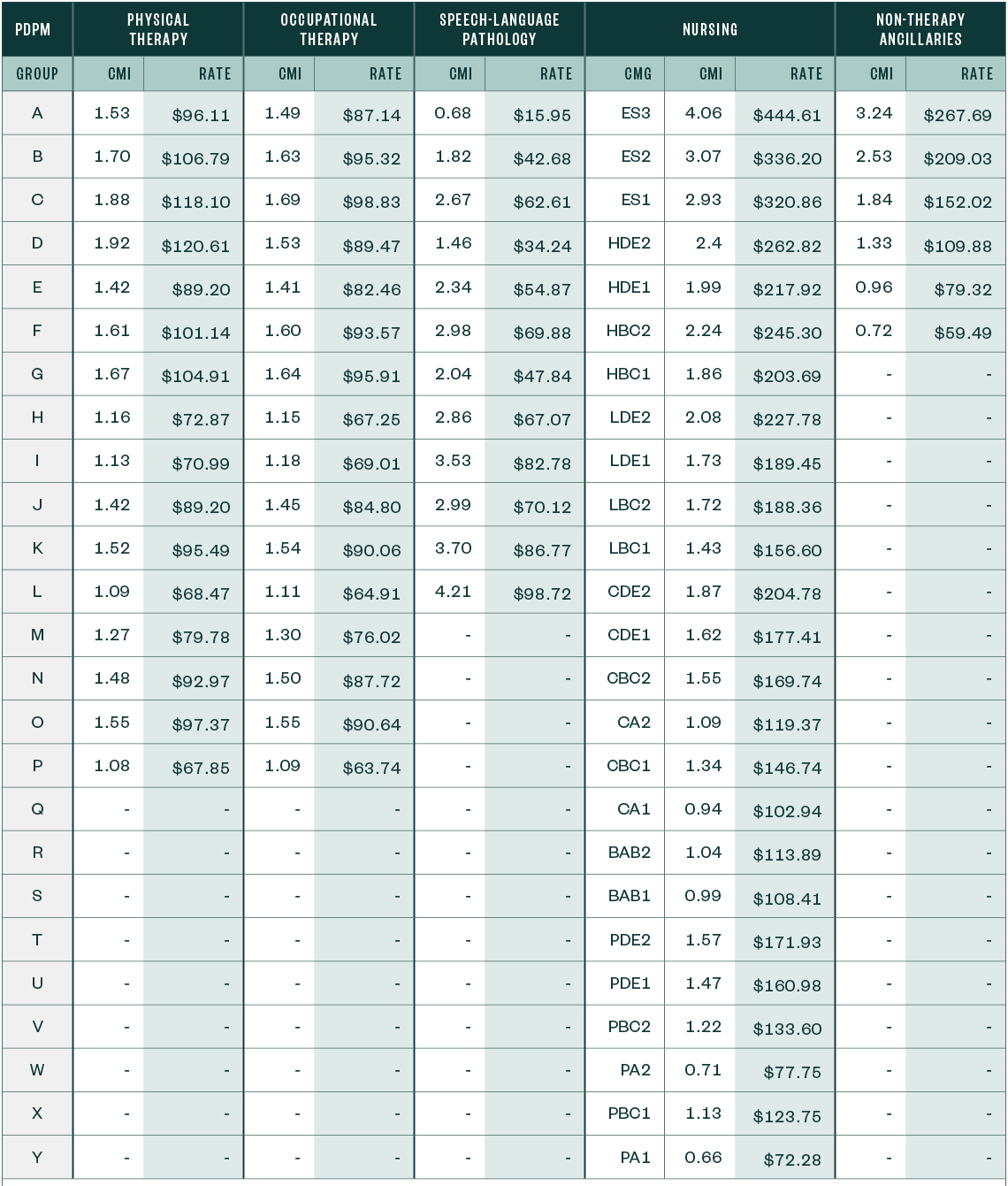
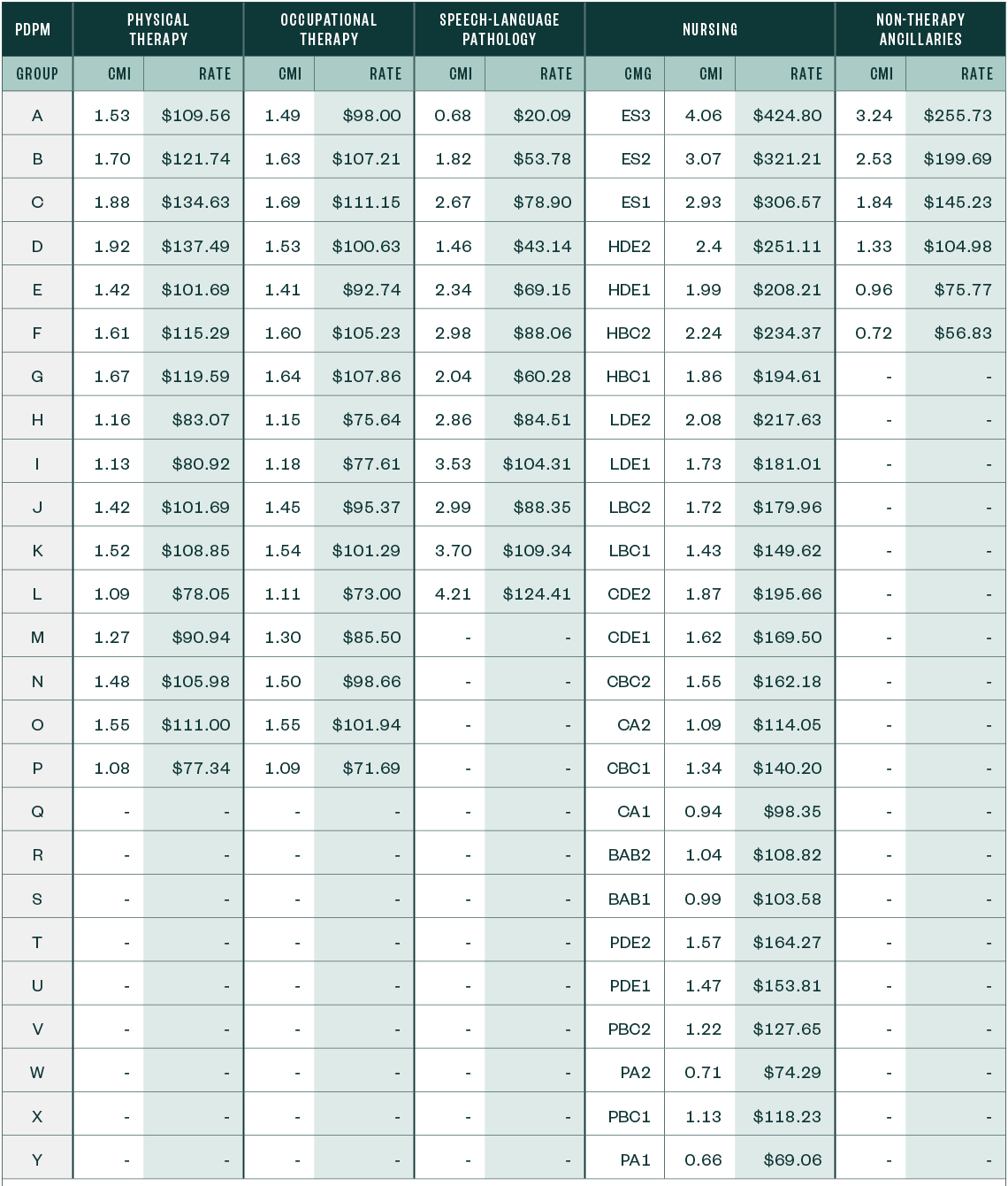
Below are the unadjusted case-mix updates for FY 2022, compared to those of the prior year, and the detailed listing of case-mix adjusted rates for FY 2022 by PDPM group.
FY 2021 Unadjusted Federal Rate Per Diem—Urban
FY 2021 Unadjusted Federal Rate Per Diem—Rural
FY 2022 Unadjusted Federal Rate Per Diem—Urban
FY 2022 Unadjusted Federal Rate Per Diem—Rural

PDPM Case-Mix Adjusted Federal Rates and Associated Indexes—Urban
PDPM Case-Mix Adjusted Federal Rates and Associated Indexes—Rural
Other Notable Updates
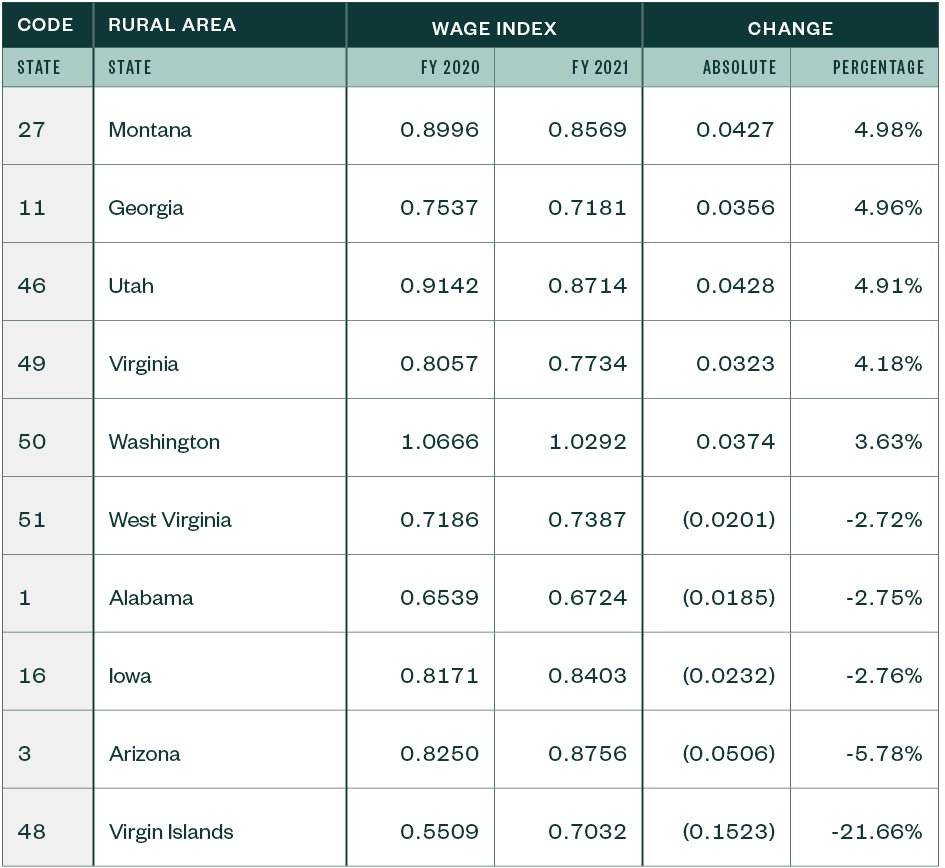
Wage Index Updates and Core-Based Statistical Area Designation
The FY 2022 SNF PPS final rule adopts the most recent Office of Management and Budget (OMB) Core-Based Statistical Area (CBSA) delineations.
The top five rule increases and decreases for urban and rural CBSAs follow.
CBSA Changes for Urban Areas

CBSA Changes for Rural Areas
Patient-Driven Payment Model Clinical Diagnosis Mappings
Through the finalized FY 2022 SNF PPS rule, CMS continues to refine the ICD-10 (International Classification of Diseases) diagnosis mappings in the PDPM.
When CMS implements sweeping changes, such as the transition from the historical Resource Utilization Grouping (RUG)-IV payment system to the PDPM model, it has authority to make changes prospectively only and will continue to do so annually as claims information validates or disputes assumptions made in its modeling.
After reviewing the FY 2020 data to compare PDPM reimbursement to the RUG-IV reimbursement to determine any needed adjustment, CMS found that it necessitated a 5% decrease in PDPM reimbursement.
When considering how to accomplish this adjustment, CMS looked at applying the entire 5% to the updated rates or to phase it in.
Due to COVID-19, CMS will wait and monitor available data for developing the FY 2023 reimbursement data. Therefore, the FY 2021 ICD-10 diagnosis mappings will stay the same.
SNF Value-Based Purchasing
Other provisions of the final rule include updates to the SNF VBP Program and follow below.
Due to the public health emergency and its effect on the readmission rates, CMS chose to suppress the SNF 30-Day All-Clause Readmission Measure (SNFRM) from the 2022 reimbursement calculation.
This achieves the following:
- VBP won’t impact low-volume providers—fewer than 25 stays—and they won’t have adjustments to their payment.
- Providers with more than 25 stays will receive back 60% of the 2% withheld regardless of previous performance measures. The updated reduction will be set at 0.8% of providers rates.
Economic Impact
The overall economic impact of this final rule is an estimated $410 million in increased payments from the US federal government to SNFs during FY 2022.
Next Steps
Providers need to review whether they have loaded appropriate SNF rates into the patient accounting system they use to bill Medicare on or after October 1, 2021.
Once the providers incorporate the revised rates, they can use best practices to validate that the rates calculate appropriately. They can accomplish this by pulling a paid claim and running it through the SNF pricer downloadable from the CMS website.
We’re Here to Help
For more information about the final rule or assistance during the course of your validation review, contact your Moss Adams professional.