
The COVID-19 pandemic public health emergency (PHE) expired on May 11, 2023—more than three years after it was first declared. Some PHE changes, like COVID-19 vaccine access, will remain. Others, like Medicaid continuous enrollment, will fade out. The potential impact of multiple revenue and compliance implications, covering everything from coding and billing to a shifting payer mix, should therefore be considered.
Hospitals will need to reassess nearly every business function for potential impacts, and health care leaders will need to break through silos and engage with trusted partners to mitigate risk and manage disruptions as they navigate change. Below are some areas where health care organizations can expect to see impacts and some steps to follow in preparation.
Medicaid Redetermination
Medicaid redeterminations have resumed with the ending of continuous enrollment. The federal payments that were incentivizing continuous state enrollment are phasing out through the end of 2023, starting with the 6.2% Federal Medical Assistance Percentage (FMAP). Medicaid populations in some states may lose coverage before others, like Florida, where roughly 250,000 people—many of them children—have already been terminated from their health plans.
While hospitals are likely to have prepared for more obvious revenue, reimbursement, and human impacts, some potential consequences may be less anticipated.
Employer Health Insurance
Some organizations may assume that when patients move from Medicaid to commercial employer-sponsored plans, hospital revenue will inevitably benefit, which could prove false if people move to plans with more expensive cost-sharing.
While the expected migration of 9.5 million people from Medicaid to employer health insurance on a claim-by-claim basis could seem like a potentially positive outcome, this would only apply when insurance is not only paying, but paying at a higher rate than Medicaid after factoring in uncollectible patient liabilities. Increasing numbers of self-pay patients could also lead to an increasing number of patients delaying care.
Less favorable instances could include people on employer or exchange plans with such high deductibles, coinsurance, and copayments that health care services would essentially become self-pay. Some patients may be unenrolled for administrative reasons, while still meeting Medicaid criteria.
It’s incumbent on providers to not only educate patients about the redetermination process, but also to proactively engage with those being disenrolled to remedy enrollment issues before they seek care and prevent them from delaying care because they believe they’re no longer covered.
Drug Pricing Program (340B) or Disproportionate Share Hospital Program (DSH)
As patients fall off Medicaid rolls, the result can potentially skew an organization’s DSH calculations, perhaps making previously eligible hospitals become newly ineligible for both the 340B and DSH. This of course would also impact a hospital’s distribution from the uncompensated care pool. These and other warnings exemplify the risks of making decisions in a silo.
As you plan your post-redetermination path, engage departments organization-wide to assess impacts and lessen surprises. One team’s change may affect another’s, so alignment is critical.
Operational, Training, and Staffing Impacts
PHE changes are expected to have far-reaching operational impacts. The sprawling implications from redetermination to telehealth flexibilities and beyond require a reassessment of staffing, system configurations, and charge capture processes.
1135 Waivers
The US Department of Health and Human Services gave providers the flexibility to waive certain Medicare, Medicaid, Children’s Health Insurance Program (CHIP), or HIPAA requirements, referred to as 1135 waivers, which will be expiring at various times as the PHE ends.
Health care providers may be subject to civil and administrative sanctions and penalties for noncompliance, so it’s important to have a good tracking mechanism to outline varying 1135 waiver expirations and individuals actively monitoring the organization’s progress as well as monitoring for changes or extensions.
Staffing Challenges
These and other challenges could leave provider staffing facing unpredictable difficulties. Consider what policies and procedures may need to be reviewed and updated to account for new processes—mainly, who will be doing this work and how they’ll be trained. Staff will need to be able to effectively perform these new processes. Training will be essential for workers to adapt to the additional wave of complexities from PHE.
Evolving Training Needs
Ongoing labor shortages could cause training hours to exceed what organizations can handle. For example, the flexibility that waived medical record request fulfillment timeliness requirements would revert to its original 30-day window. Health care providers will need to be appropriately staffed and trained to accommodate that change.
Medicaid redeterminations can have similar staffing and training impacts as hospitals work to identify those affected before getting overwhelmed with lost coverage cases. Patient-access staff, particularly financial counseling, could be greatly affected, considering that many patients will have just lost coverage. A lot of this staff will need retraining for their evolving roles.
Capacity Management to Address Labor Impacts
Appointing an individual in a full-time capacity management leadership role to oversee labor demands can help to provide structure in this area. A capacity management committee can also deliver value to prioritize work and commitment around key areas such as entry, care delivery, and discharge.
Impacts on Other Workflows
The end of the PHE coincides with other developments that affect workflows, including the good faith estimates (GFE) requirement for the No Surprises Act (NSA) and Centers for Medicare and Medicaid Services (CMS) Transmittal 18.
Additional operational focus areas persist, such as the need to improve revenue integrity, improve supply chains, and reduce hospital-acquired infections. Concurrent activities may also be exacerbating revenue and compliance impacts that have already been impacted by the PHE. Beyond needing to adjust workflows in response to new developments, reevaluating responses to past changes may also be in order, such as with the NSA.
Work queues created to support GFE-related compliance around some of the GFE components might not populate all the items as expected, leading to missed or improperly prepared items. Processes could have been rolled out across different departments at different times.
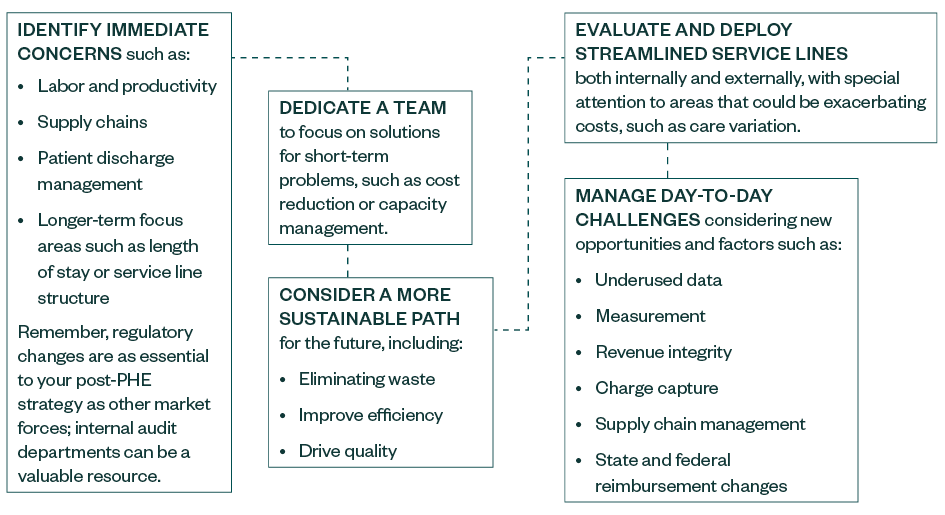
How to Prepare for Transitions
Health care leaders could benefit from taking a proactive and disciplined approach toward efficiency and cost-containment strategies, revenue maximization, and sustainable transformation. Consider this blueprint:
Conduct Thorough Assessments
Some waivers expired as soon as the PHE ended. Other waivers, like payment parity for telehealth services, will remain until the end of 2023. Still others, like Medicaid continuous enrollment, will fade out gradually on a state-by-state basis.
No matter where your organization falls in its readiness for this road ahead, the complexity of this era will create challenges for even the most prepared health care systems—especially as they unfold concurrently with other major developments such as the NSA. With risks of domino effects, stay watchful for unexpected impacts and siloed reactions that can jeopardize operations.
Legislation is still ongoing, so an agile organization that’s prepared to pivot as needed may be more able to adapt to circumstances such as changes slated for discontinuation ending up continued after all.
We’re Here to Help
For more information on the challenges facing the post-PHE era in health care, please contact your Moss Adams professional.