
The COVID-19 pandemic disrupted nearly every aspect of the health care industry with implications for care delivery across the continuum.
Below are highlights of the impacts on patients, providers, and health plans, as well as opportunities to stabilize and redesign primary care delivery in response.
Implications
For Patients
- Trust Issues. Health care consumers’ trust in care delivery has been shaken, causing them to postpone preventive care and health maintenance, delay elective procedures, and avoid emergency and urgent care settings.
- Children’s Physical, Mental, and Dental Health. Data shows a sharp decrease in childhood vaccine administration, which leaves young people exposed to vaccine-preventable diseases; furthermore, the urgency for catching up will increase quickly as social distancing relaxes. These vulnerabilities aren’t limited to physical health, but also include behavioral and dental health. The Centers for Medicare & Medicaid Services reported that children enrolled in Medicaid and CHIP received 44% fewer outpatient mental health services and 69% fewer dental services in a three-month period in 2020 compared to the same period in 2019.
- Senior Care. Data also shows that one in three seniors are delaying or avoiding any medical care due to concerns related to COVID-19, which leaves older populations with larger percentages of chronic disease vulnerable to preventable acute episodes of care.
For Providers
- Added Stressors. Providers must adapt care delivery processes to ensure safety while delivering needed services under mounting financial pressures.
- Missed Benchmarks. Healthcare Effectiveness Data and Information Set (HEDIS) measures are in decline as a result of suspended primary care visit-linked health maintenance.
- Shifts from In-person Visits. The primary care delivery model—and its foundations in relationship-based care—has been eclipsed by the necessary transition to televisits, accelerating the adoption of this technology and replacing in-person visits at never-before-seen rates.
For Health Plans
- Lapses in Prevention and Wellness Visits. Delayed health maintenance may require more expensive interventions in the future, creating risk to payers beyond the savings generated by reduced volume in 2020.
- Coverage Shifts. A rise in unemployment as well as further pressure on employer-based plans is likely to fuel the shift to a capitated, or value-based, model of payment.
- Care Avoidance. As patients defer care for acute conditions due to COVID-19 exposure, rates of acute non-elective hospitalizations have reduced.
- Delayed Care. At the same time and for the same reasons, preventable hospitalizations, or ambulatory care-sensitive conditions, are also on the rise.
Find Opportunity in Disruption
This disruptive period provides a rare opportunity for health plans and providers to partner in targeted areas of benefit to members, patients, and communities.
In particular, working together to strengthen patients’ sense of value and trust in preventive and chronic care while maintaining COVID-19 safety precautions will be critical to reducing preventable morbidity and mortalities, as well as unnecessary costs.
With a focus on lean methodologies and continuous improvement, partnerships work when problems are jointly defined and agreed upon, and strategies and tactics are developed and executed at the appropriate level of delivery.
In an effective lean management system, consensus starts with understanding the problem to be solved and the collective and organizational benefits—or what’s in it for me (WIIFM)—are transparent.
Leadership decisions determine the what. The how, then, should be determined by those closest to the work, namely managers and front-line staff, with cascaded metrics to align the organizations and the partnership as a whole.
An elemental lean management structure such as this can be implemented even as the pandemic continues, helping your organization restart, enhance, and redesign care processes to:
- Prevent delays in services and deliver timely care for chronic conditions like high blood pressure, cholesterol, and heart disease
- Stave off worsening health, hospital admissions, and emergency department visits
- Stabilize operations and bring productivity back online
Improvement Workshops and Leadership Coaching
The urgent priority of many health care organizations is to stabilize operations and get productivity back online safely. This can be facilitated with straight-forward strategies that require process improvement and daily management fueled by the problem-solving talents of those workers on the front line of care.
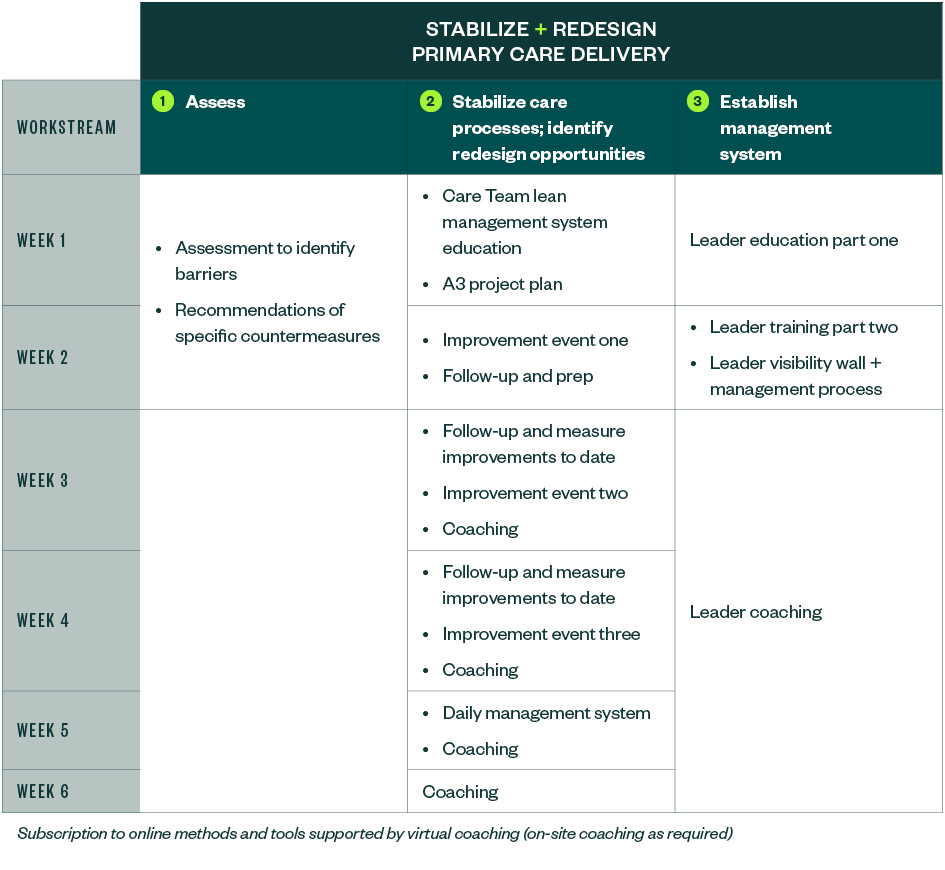
The approach for each organization varies depending on the size of its operations and unique needs. Below is a sample approach to help stabilize and redesign your primary care delivery.
We’re Here to Help
To learn more about how your organization can improve its processes to regain patient trust, prevent delayed services, and increase productivity, contact your Moss Adams professional.