
A version of this article previously ran in the March 2021 edition of Healthcare News.
In response to the COVID-19 pandemic, telemedicine took a dramatic leap forward as organizations sought rapid implementation to continue providing services among lockdowns and social distancing protocols.
While the shift from face-to-face (F2F) visits to virtual care—via both phone and video—provides some conveniences, inevitable obstacles emerged for health systems, and challenges continue to mount as adoption of telemedicine becomes widespread.
Employing problem-solving solutions through lean methodologies, however, can help counter workflow impediments that carry over from in-person visits—as well as any potential erosions to efficiencies—so your organization can make the most of virtual delivery methods and provide high quality care.
Telemedicine Challenges
Health care organizations face hurdles in several areas related to telemedicine.
Technology and Connectivity
Software and application platforms can present technical obstacles such as limited Wi-Fi and cabling in old clinics, and even basic hardware barriers like laptops with insufficient video capabilities.
Many patients also don’t have access, affinity, or skills to manage virtual platforms, and medical groups don’t have time or experience to train patients in these capacities.
Appropriate Use
Certain conditions might not be safe and logical for virtual care.
While metabolic conditions and behavioral health may be logical fits for virtual visits, exam-dependent conditions may not fit.
For example, consider the need for serial neurologic exams for patients with Parkinson’s Disease, magnified exams performed in ENT practices, and common musculoskeletal exam maneuvers, as well as the essentials of the bimanual pelvic exam.
Auscultation-dependent pulmonologists, primary care providers, and cardiologists will need remote auscultative devices that integrate with electronic health records (EHRs) for accuracy.
Visit Utilization
Depending on the specialty, there’s the uncomfortable and sometimes predictable dilemma that many virtual visits only precipitate a F2F visit—potentially using up access to care at twice the rate.
In addition, these visits might be initially shorter and more efficient, but over time become swamped by agendas.
Pre-existing Issues
Existing problems within an organization often won’t be solved with new setups. The same problems that exist during in-person visits are likely to persist in new platforms, including workflow and cycle time challenges.
These could include:
- Clogged EHR InBasket
- Batched work after hours
- Reduced wellness and preventive care capacity
- Continued challenges with complex visits
3 Steps to Improvement
Lean methodologies offer countermeasures to these dilemmas, helping you identify problems and streamline and perfect new processes while improving existing ones.
Organizational learning and adoption of lean methods can then help bring sustained success into the future as the health care landscape continues to change.
1. Identify and Understand Problems
First, it’s important that your teams define the root cause of challenges to propose countermeasures, set metrics, and test solutions.
This can be done through the critical thinking process known as A3 thinking—named for the large size of paper used as a tool during the planning process.
This structured method provides a way to analyze causality of problems and set targets to test solutions—which can ultimately enable you to plan your care transformations from the executive level down to point-of-care teams.
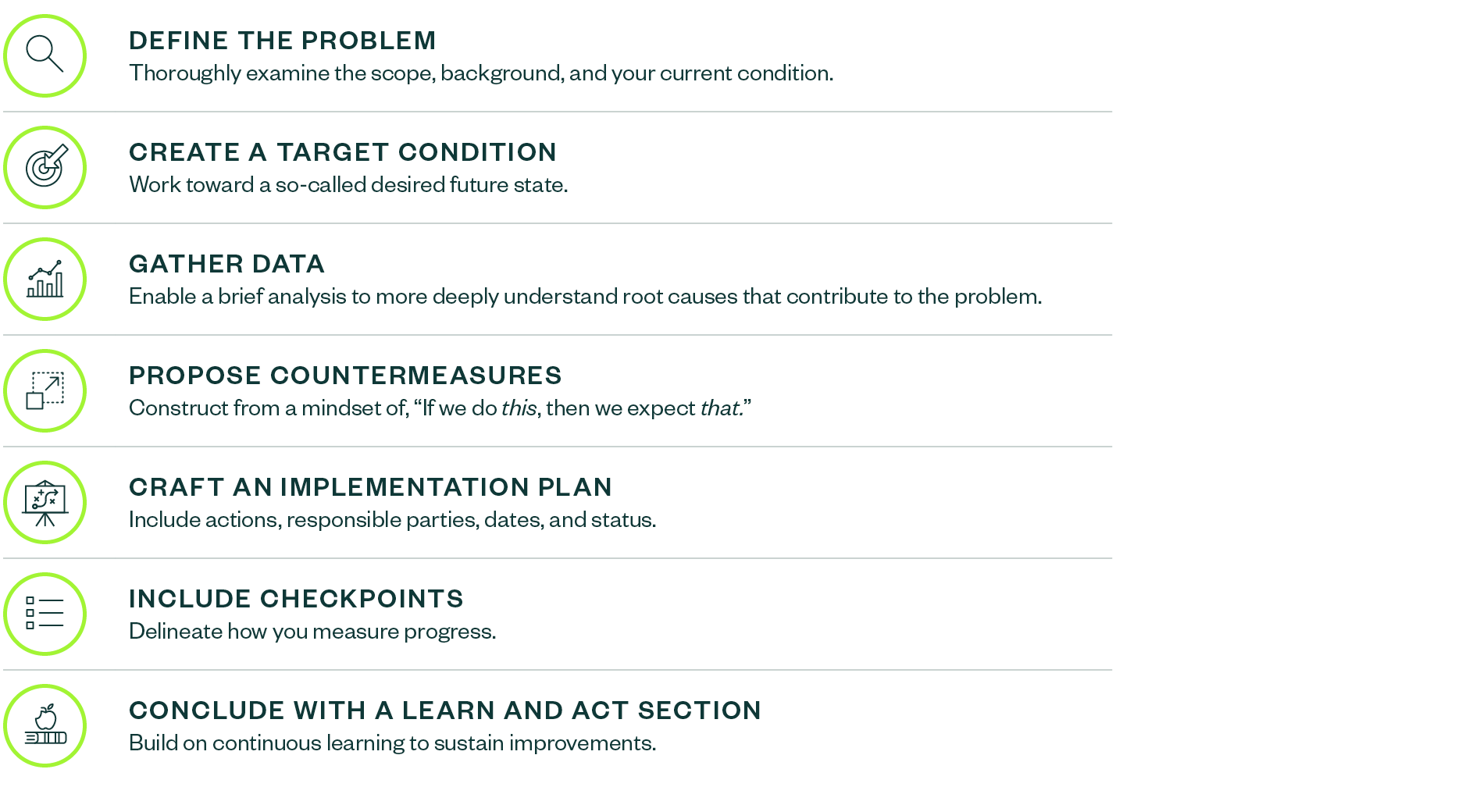
Creating an A3 guide can help you define your problem, craft countermeasures, test solutions, and sustain improvements.
To create an A3, you:
.png?width=1890&height=1040&ext=.png)
A3 guides should be created for your executives, as well as any teams who will undertake the improvement work at the point of care.
Targets for the frontline improvement teams should be the process measures that enable the outcomes the executives strive toward. These are called linked metrics. Without strongly linked metrics, linear progress is less likely.
2. Map Care Processes
When current processes are dysfunctional, you can map them to expose steps in care that need improvement. This learning method and skill is known as value stream mapping.
Mapping virtual care in the current hasty-and-flawed state enables a vision of the mistake-proofed near future state. Details such as time and where defects reside in the patient’s journey can expose the gaps in quality from which you derive targets for improvement.
3. Test Change Cycles to Improve Processes
The next step involves creating a plan and timeline for target-specific Plan-Do-Check-Act (PDCA) cycles performed by the people who know the work and adopt the changes.
If a PDCA fails, it can become a learning experience, allowing you to question what about the test failed and what can be modified to test again.
A flawed PDCA shapes the next round, iterating toward success at the point of care. Measuring time and defect reduction in each PDCA reveals what might be proper sequences of F2F and virtual visits for new, return, and complex patient care.
Performing tests with actual IT and delivery team members can help lead to practical implementation. You can organize training facilities into simulation labs for PDCA before you deploy ideas and care models on production mode in the EHR.
The simulated experiences also inform the training methods you’ll need to spread capabilities across teams. Realistic implementations can then ensue.
Improvement Solutions
As your organization’s leaders learn lean methods, your teams will:
- Identify gaps between usual processes and virtual processes, as well as your current state and future state—finding innovative solutions to close gaps and transform processes
- Defend your teams against burnout and administrative burden within this new service delivery platform by emphasizing time with patients through reducing waste-ridden processes
- Embrace the call to service to improve patient care through innovative new care methods
We’re Here to Help
To learn more about how your organization can enhance its telemedicine services, contact your Moss Adams professional.